Sanatoriums closed primarily due to changes in mental health care approaches, costs, and societal values. The invention of antipsychotic drugs enabled outpatient treatment, reducing the need for long-term institutionalization. Additionally, inpatient care was costly, often ineffective, and faced criticism regarding patients’ rights.
In the 1970s, films such as One Flew Over the Cuckoo’s Nest highlighted mistreatment in mental health institutions. This influenced public opinion and policy toward deinstitutionalization. Governments shifted funding away from inpatient facilities to community-based outpatient programs. Psychiatric hospitals transitioned into acute care centers, handling short-term crises rather than lifetime stays.
Concerns about human rights also played a role. Reports of political abuse of mental health commitment, particularly in communist countries, raised alarms about institutionalization as a violation of individual freedom. As a result, many patients previously housed in sanatoriums were released into community care settings.
Patient outcomes vary significantly after sanatorium closures. Some receive consistent outpatient treatment and family support. For example, one patient may live with relatives who monitor his condition. Another avoids family contact for safety reasons and moves between furnished apartments with minimal supervision. Compliance with medications and therapies remains challenging.
Sadly, others reject treatment entirely and face homelessness. Some rely on alcohol or other substances to self-medicate. This group often experiences vagrancy and lacks stable living conditions. The transition from institutional care to community life has been uneven, with gaps in support services and follow-up.
- Sanatorium closures linked to medication advances and cost concerns.
- Public opinion shifted against long-term institutionalization in the 1970s.
- Hospitals refocused on short-term acute psychiatric care.
- Patients live in varied settings: with family, in apartments, or homeless.
- Compliance with outpatient treatment is inconsistent.
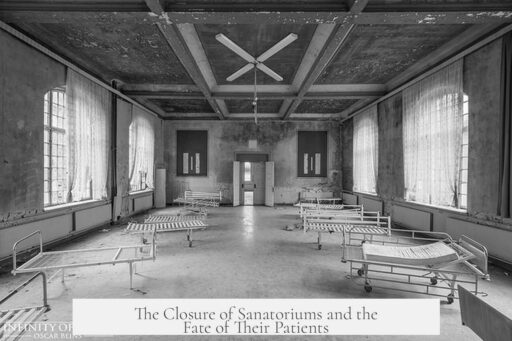
Why Were Sanatoriums Closed Down, and What Happened to All the Patients?
Sanatoriums closed down primarily because society shifted away from long-term institutional care towards outpatient treatment, driven by changing perceptions, medical advancements, and economic factors. But what exactly sparked this massive change? And after the doors were shut, where did the patients go? Let’s pull back the curtain on this pivotal moment in mental health history.
First, a quick peek into the 20th century. Sanatoriums, or psychiatric hospitals, were once the go-to solution for chronic mental illness. Yet by the 1970s, things were buzzing with new ideas. Movies like One Flew Over the Cuckoo’s Nest painted a grim picture of life inside these institutions. Electroshock therapy and strict confinements looked less like treatment and more like punishment on the big screen. This negative portrayal stirred public sentiment. Suddenly, mental hospitals seemed not only harsh but unkind and uncaring.
Alongside this shift in perception came hard numbers—money matters. Inpatient care was expensive. Governments and health systems found funding long-term care costly. But more than just budget woes, many professionals questioned effectiveness. Was locking people away for months or years really helping? For chronic cases, the evidence suggested otherwise. In fact, some argued that keeping patients institutionalized could be downright counterproductive, hindering their path back to normal life.
Human rights concerns added fuel to the fire. The Cold War era revealed unsettling abuses in Communist countries, where mental health commitments became a weapon of political repression. This alarmed many and raised ethical questions worldwide. Institutionalizing someone without solid grounds felt like violating their core rights. It was clear a new approach was needed.
Then came the game changer: antipsychotic drugs. These medications, developed in the mid-20th century, enabled many patients to manage symptoms outside hospital walls. Suddenly, long-term confinement wasn’t the only option. Treatment could shift to outpatient settings—cheaper, less restrictive, more humane.
With this medical breakthrough, funding priorities flipped. State resources flowed into community-based outpatient programs instead of sprawling psychiatric hospitals. Institutions that once housed hundreds became acute care facilities, focusing on short-term crises instead of lifelong care.
So, what happened to all the patients? The mass closure of sanatoriums, sometimes called deinstitutionalization, thrust many individuals back into communities. This transition hasn’t been smooth or uniform. Some patients receive ongoing outpatient care, attend therapy, and maintain medication regimens. Others struggle with access, compliance, or support.
Consider three patient stories that capture the variety of outcomes:
- One lives with family, benefiting from direct support and supervision. This setup helps stabilize daily life and treatment adherence.
- Another avoids family for safety reasons and moves through a series of furnished apartments. Despite some independence, his family tries to keep tabs, though he occasionally disappears without explanation for weeks.
- The third refuses formal treatment entirely. He self-medicates with alcohol and has become nearly a full-time vagrant, highlighting how some fall through the cracks.
These examples reveal the tough reality behind the headlines. While deinstitutionalization intended to promote freedom and dignity, it sometimes resulted in inadequate care. Many communities weren’t prepared for the influx of patients needing support. Without stable housing, mental health services, or continuous supervision, some individuals faced homelessness or worsening symptoms.
So, was closing sanatoriums a good move? It’s a complicated question. On one hand, it ended a system marked by cruelty and neglect. Patients gained personal freedoms once denied. Treatment became more modern and less reliant on confinement.
On the other hand, the transition exposed gaps in social services and mental health infrastructure. The promise of community care often fell short due to insufficient funding or planning. Patients left the institutions but not always the challenges. Many still struggle with medication compliance, housing, and employment. Mental illness doesn’t magically vanish outside hospital walls.
Today, the legacy of sanatorium closures pushes us to ask hard questions:
- How can we balance patient rights with effective care?
- What safety nets and services truly help former patients thrive in communities?
- Are outpatient programs adequately funded to prevent homelessness and relapse?
These questions remain vital. Mental health care continues to evolve, learning from past mistakes and successes alike. Deinstitutionalization sparked a revolution, but it also taught the importance of comprehensive, compassionate care both inside and outside hospital walls.
In a nutshell, sanatoriums were closed because treating mental illness no longer meant locking people away. Medical advances, economic realities, and human rights transformed care models. Patients—now living in communities—experience diverse outcomes, influenced by support systems and personal circumstances.
Perhaps one day, we will achieve a world where no patient fades into obscurity on the streets or cycles endlessly through shelters. Until then, the story of sanatorium closures reminds us of progress’s complexities and the ongoing fight for mental health reform.
Why were sanatoriums closed down?
Sanatoriums closed mainly because inpatient treatment was costly and often ineffective. New antipsychotic drugs allowed outpatient care. Also, concerns about human rights and negative public views pushed for deinstitutionalization.
What role did antipsychotic drugs play in closing sanatoriums?
These drugs let patients manage symptoms outside hospitals. This shifted care from long stays to outpatient treatment, reducing the need for large institutional settings.
What happened to patients after sanatoriums shut down?
Many patients moved into communities with varying support. Some live with family, others in apartments or homeless. Treatment compliance differs widely among them.
Were all former patients able to get outpatient treatment?
No, some receive regular treatment, but others refuse it or self-medicate. This results in some becoming homeless or living unstable lives.
How did society view long-term psychiatric hospitals before closures?
They were often seen as inhumane and ineffective. Media like movies showed harsh treatments, influencing public opinion to favor less restrictive alternatives.